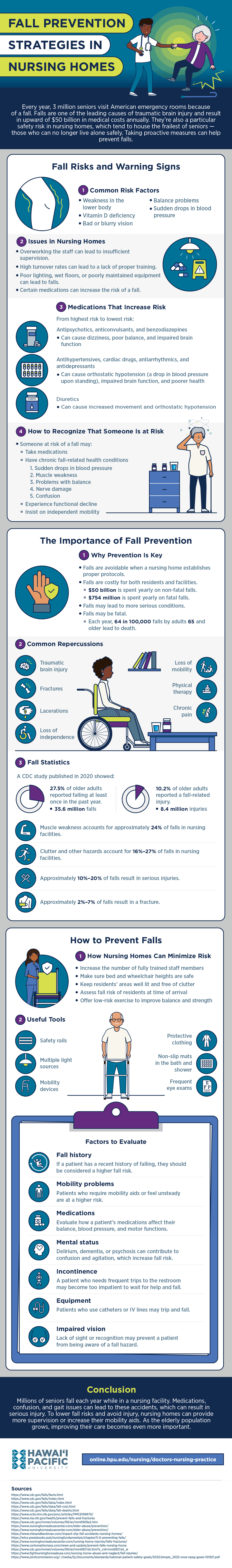
Fall Risks and Warning Signs
There are common factors and warning signs that indicate someone may be at risk for a fall. Knowing and looking out for these signs may help avoid them.
Common Risk Factors
Many falls are caused by weakness in the lower body, which often results from inactivity, medical conditions, or previous injuries. Other common risk factors include vitamin D deficiency, bad or blurry vision, and balance problems. If a patient experiences sudden drops in blood pressure, they may be at higher risk of a sudden fall.
Issues in Nursing Homes
In addition to medical causes, conditions in nursing homes can make falls more likely to occur. For example, an overworked staff is unlikely to provide sufficient supervision, and high turnover rates can lead to deficient training. If the facility has poor lighting, wet floors, or poorly maintained equipment, the risk of falling increases.
Medications That Increase Risk
Certain medications can also increase an individual’s fall risk. Most fall within three categories, which are listed below from highest risk to lowest risk.
Antipsychotics, Anticonvulsants, and Benzodiazepines
These medications can cause dizziness, poor balance, and impaired brain function.
Antihypertensives, Cardiac Drugs, Antiarrhythmics, and Antidepressants
These medications can cause orthostatic hypotension (a drop in blood pressure upon standing), impaired brain function, and poorer health.
Diuretics
These medications can cause increased movement and orthostatic hypotension
How to Recognize That Someone Is at Risk
Someone at risk of a fall may take medications or have chronic fall-related health conditions such as sudden drops in blood pressure, muscle weakness, problems with balance, or nerve damage. Individuals experiencing prolonged confusion are at higher risk for a fall. If someone is experiencing functional decline but insists on independent mobility, they should be monitored to ensure they don’t fall.
The Importance of Fall Prevention
If a patient is protected before they fall, they can avoid serious injury.
Why Prevention Is Key
Establishing proper protocols can help nursing homes avoid falls, which are costly for both residents and facilities. The CDC reports that $50 billion is spent yearly on non-fatal falls, and $754 million is spent yearly on fatal falls. Each year, 64 in 100,000 falls by adults 65 and older lead to death. Non-fatal falls may lead to more serious conditions.
Common Repercussions
One of the more serious repercussions is traumatic brain injury. Falls may cause fractures, lacerations, and chronic pain. They may lead to a loss of mobility and independence for the patient. Often, those who fall require physical therapy.
Fall Statistics
A CDC study published in 2020 showed that 27.5% of older adults reported falling at least once in the past year, amounting to 35.6 million falls. Furthermore, 10.2% of older adults reported a fall-related injury, amounting to approximately 8.4 million injuries.
Muscle weakness accounts for approximately 24% of falls in nursing facilities. Clutter and other hazards account for 16%-27% of falls in nursing facilities. Approximately 10%-20% of falls result in serious injuries, and approximately 2%-7% of falls result in a fracture.
How to Prevent Falls
Nursing homes can take steps to minimize fall risk for their patients.
How Nursing Homes Can Minimize Risk
One step nursing homes can take to minimize their patients’ fall risk is to increase the number of fully trained staff members and reduce the stress placed on staff. Homes can make sure bed and wheelchair heights are safe and keep residents’ areas well lit and free of clutter. Patients should be assessed for risk at the time of their arrival to the facility. Homes can also offer low-risk exercise to improve balance and strength.
Useful Tools
Nursing homes can add physical tools to improve patients’ quality of life. For example, safety rails, mobility devices, and non-slip mats in the bath and shower provide support for mobile patients. Installing multiple light sources and offering frequent eye exams reduce patients’ risk of falling due to being confused and unaware. Higher-risk patients can wear protective clothing, such as padded garments and supportive shoes.
Factors to Evaluate
Because assessment and personalized care are critical to preventive strategies, nursing homes should be aware of risk factors during their evaluations.
Fall History
If a patient has a recent history of falling, they should be considered a higher fall risk.
Mobility Problems
Patients who require mobility aids or feel unsteady are at a higher risk.
Medications
Evaluate how a patient’s medications affect their balance, blood pressure, and motor functions.
Mental Status
Delirium, dementia, or psychosis can contribute to confusion and agitation, which increase fall risk.
Incontinence
A patient who needs frequent trips to the restroom may become too impatient to wait for help and fall.
Equipment
Patients who use catheters or IV lines may trip and fall.
Impaired Vision
Lack of sight or recognition may prevent a patient from being aware of a fall hazard.
Creating Safer Nursing Homes
Millions of seniors fall each year while in a nursing facility. Medications, confusion, and gait issues can lead to these accidents, which can result in serious injury. To lower fall risks and avoid injury, nursing homes can provide more supervision or increase their mobility aids. As the elderly population grows, improving their care becomes even more important.
Sources
The Carson Law Firm, "How to Prevent Falls in a Nursing Home"
CDC, Cost of Older Adult Falls
CDC, Deaths From Fall-Related Traumatic Brain Injury
CDC, Deaths From Older Adult Falls
CDC, Facts About Falls
CDC, Older Adult Falls Data
CDC, Older Adult Falls Prevention
CDC, "Trends in Nonfatal Falls and Fall-Related Injuries Among Adults Aged ≥65 Years"
Fight Nursing Home Abuse, "Fall Injuries"
Joint Commission, Home Care National Patient Safety Goals
National Institute on Aging, "Prevent Falls and Fractures"
National Library of Medicine, "Traumatic Brain Injury in Older Adults: Do We Need a Different Approach?"
Nursing Home Abuse Center, "Elder Abuse Prevention"
Nursing Home Abuse Center, "Falls & Fractures in Nursing Homes"
Viles & Beckman, LLC, "The Impact of Slip and Fall Accidents in Nursing Homes"
Wisconsin Technical College System, 5.6 Preventing Falls